In her article entitled The Puzzle of Endometriosis, Ballweg quotes a colleague who describes endometriosis as ‘a riddle, wrapped in a mystery inside an enigma’. In the decades following the publication of her article, it seems as though little has changed, and endometriosis is still a misunderstood disease.2

Endometriosis affects ~10% of women of reproductive age and is the cause of between 35% and 50% of infertility. The main symptoms include intense dysmenorrhea (severe and frequent menstrual cramps and pain during menses), dyspareunia (persistent or recurrent genital pain that occurs just before, during or after intercourse) and chronic pelvic pain. It takes on average seven years a diagnosis is confirmed.1
Endometriosis is characterised by the development and presence of histological elements like endometrial glands and stroma in anatomical positions and organs outside of the uterine cavity.3
Women’s experiences of endometriosis
Gremillet et al recently published the findings of their qualitative study, which explored the impact of severe endometriosis on the professional lives of women living with infertility.1
Pain is the most prominent symptom, hindering work and leading to a substantial reduction in effective work hours. Digestive and urinary problems, along with heavy bleeding, contribute to frequent work interruptions. The cyclical and unpredictable nature of symptoms causes difficulty in concentration, chronic fatigue, anxiety, and irritability.1
Many women choose not to disclose these challenges to employers and colleagues due to fear of judgment and negative reactions. Privacy preservation, better information dissemination, and self-protection are key motivators for those who do decide to share their experiences.1
Often, such revelations are made discreetly during off-the-record meetings with superiors, with women feeling it more legitimate to justify absences by medicalising their infertility.1
This disclosure is seen as a pivotal moment in their professional lives, fostering understanding and support from their professional environment, ultimately making work more manageable.1
Pathogenesis of endometriosis
A definitive diagnosis of endometriosis is mainly based on surgical findings. Dependence on symptoms that require surgery, may be at the root of delayed diagnosis in many cases.4
Early diagnosis is vital to protect fertility, especially in light of the impact of age on ovarian reserve (the reproductive potential left within a woman's two ovaries based on number and quality of eggs).4
Understanding the pathogenesis of endometriosis plays a crucial role in decisions regarding clinical and therapeutic interventions. Some of the most popular theories regarding the pathogenesis of endometriosis include:4
- The retrograde menstruation theory, proposed by Sampson in 1927, suggests that viable endometrial tissue moves into the pelvic cavity during menstruation, adheres to peritoneal cells, and invades structures, explaining endometriosis. Early menses onset, heavy menstrual flow, and anatomical predominance on the right side support this theory.
- The coelomic metaplasia and mullerian remnants hypotheses propose in situ origin from embryological remnants.
- Sampson's hematogenous and lymphovascular dissemination theory suggests endometrial cell spread via vasculature, supported by murine models and clinical evidence of emboli in lymph nodes.
- The stem cell theory posits altered stem cell trafficking as key to endometriosis. Bone marrow-derived stem cells contribute to endometrial regeneration, with increased pluripotential cells in women with endometriosis during menses. These cells can differentiate into endometrial cells outside the uterus, explaining extraperitoneal endometriosis.
- Genetic factors contribute, with familial clustering and heritability estimated at 51%. Genome-wide studies link endometriosis to risk loci in sex steroid hormone pathways. In infertility, follicle-stimulating hormone beta (FSHB) and follicle-stimulating hormone receptor (FSHR variants impact hormonal profiles. FSHB and FSHR are genes associated with the production and regulation of follicle-stimulating hormone (FSH), a key hormone in the reproductive system.
- The epigenetic theory emphasises dynamic changes in chromatin structure. DNA methylation, especially in genes like homeobox gene10 (HOXA10), essential for unravelling the molecular mechanisms that govern embryonic development and for gaining insights into the origins of various congenital disorders, has been linked to impaired uterine receptivity. Aberrant DNA methylation in progesterone receptor genes contributes to persistent progesterone resistance. Histone modifications, such as hypoacetylation, occur in endometriotic stromal cells. Over 100 microRNAs are expressed in endometriotic lesions, influencing processes like epithelial-mesenchymal transition, cell proliferation, and angiogenesis. Epigenetic factors may offer diagnostic, prognostic, and therapeutic insights into endometriosis.
However, according to Bonavina et al, these theories do not explain the natural history of the disease.4
Pathophysiology of endometriosis
Pain and mechanical factors
Pain plays a crucial role in endometriosis-related infertility, affecting the possibility of intercourse. Superficial and deep dyspareunia make intercourse difficult, leading to avoidance, thus impacting conception.4
Endometriosis, particularly in severe stages, increases the risk of deep dyspareunia by 9-fold due to its effect on pelvic structures. Furthermore, endometriosis-associated pelvic pain can reduce sexual desire, and arousal. Mechanical factors like pelvic adhesions and anatomical distortion further hamper conception.4
Ovarian reserve: A key fertility prognostic factor
Ovarian reserve, a key fertility prognostic factor, is adversely affected by endometriosis, particularly in endometriomas. Ovarian reserve lacks precise predictive tools, but antral follicle count and anti-Mullerian hormone levels are widely used to determine a women’s reproductive potential.4
Endometriomas (unique cysts with no real capsule) exchange contents with the healthy ovarian cortex, inducing oxidative stress, inflammation, and fibrosis. Histopathological studies reveal reduced follicular numbers and activity in endometriomas.4
Impact of endometriosis on oocyte quality
The impact of endometriosis on oocyte quality, which is crucial for fertility preservation, is much debated. While some studies show no impact on embryo morphology, others using time-lapse technology suggest altered relative kinetics, indicating poorer embryo quality.4
Dysregulation of steroidogenesis change the follicular microenvironment, and oxidative stress in granulosa cells contribute to reduced oocyte quality. Furthermore, follicular fluid from endometriosis patients induces DNA damage in oocytes and systemic and peritoneal inflammation in endometriosis influences follicular fluid composition and damages spindle and chromosomes in oocytes.4
Gamete transport, anatomical distortions, and inflammatory microenvironments associated with endometriosis impair sperm-oocyte interaction and disrupt acrosome reactions.4
Impaired ovulation
Clinical data on spontaneous ovulation rates in women living with endometriosis are limited and contentious. Elevated prolactin levels, significantly present in these women, may contribute to anovulation by disrupting luteinizing hormone pulsatility and hindering hypothalamic function.4
Hyperprolactinaemia (elevated levels of prolactin, a hormone produced by the pituitary gland) inhibits oestrogen receptors, inhibiting ovulation. Luteinized unruptured follicle syndrome, a condition characterised by the failure of a mature ovarian follicle to release its egg (ovulate) during the menstrual cycle, even though the follicle has undergone the luteinization process, forming a structure called a corpus luteum, is another potential cause of ovulation failure.4
Women living with endometriosis may also experience altered oestrogen and progesterone patterns, compromising the luteal phase (a specific stage of the menstrual cycle that occurs after ovulation and before the onset of menstruation) and hindering ovulation.4
Endometrial receptivity
Women living with endometriosis experience reduced implantation rates in natural and assisted reproductive cycles, indicating potential defects in endometrial receptivity. The eutopic endometrium exhibits molecular and functional abnormalities.4
Furthermore, dysregulation of steroid hormone signalling, progesterone resistance, and altered hormone receptor levels contribute to impaired endometrial receptivity.4
Histological criteria for assessing receptivity have limitations, prompting a shift to molecular analyses. Dysregulated genes, including HOXA10 and integrins, crucial for implantation, exhibit altered expression in endometriosis.4
Defects in decidualisation, immune cell imbalances, and pro-inflammatory conditions further contribute to an unfavourable environment for embryo implantation.4
Adenomyosis and other uterine factors
Endometriosis frequently coexists with adenomyosis (characterised by the presence of endometrial tissue, which normally lines the uterus, growing into the muscular wall of the uterus (myometrium), especially in infertile women, and their concomitant presence may worsen fertility outcomes.4
Meta-analyses show that women with adenomyosis have lower clinical pregnancy rates, higher miscarriage risks following assisted reproductive technology (ART), and adverse pregnancy outcomes.4
How do you manage endometriosis-associated infertility?
Endometriosis currently lacks a curative treatment. Clinical management of endometriosis-associated infertility is challenging due to diverse patient phenotypes, requiring a personalised approach. Pharmacotherapy and surgical interventions are aimed at managing symptoms.4,5
Pharmacotherapy aims to reduce inflammation, suppress ovarian cycles, and inhibit oestrogen effects. Surgery may involve removing identified endometriotic lesions or complete excision of pelvic organs. Treatment decisions should be based on factors like age, ovarian reserve, infertility duration, and concomitant factors.4,5
Pharmacotherapy options include hormonal therapies inducing a hypoestrogenic state (oral contraceptives, progestins, danazol, gonadotropin hormone-releasing hormone [GnRH] agonists), as well as pain-relieving agents like nonsteroidal anti-inflammatories (NSAIDs) and opioids.5
The European Society of Human Reproduction and Embryology (ESHRE) endometriosis guideline suggests offering hormone treatment or surgery for recurrent pain in women living with endometriosis.6
Pharmacotherapy options include NSAIDs, hormone treatments (combined hormonal contraceptives, progestogens, GnRH agonists, or antagonists), and others. Shared decision-making is encouraged, considering individual factors like preferences, side effects, efficacy, costs, and availability.6
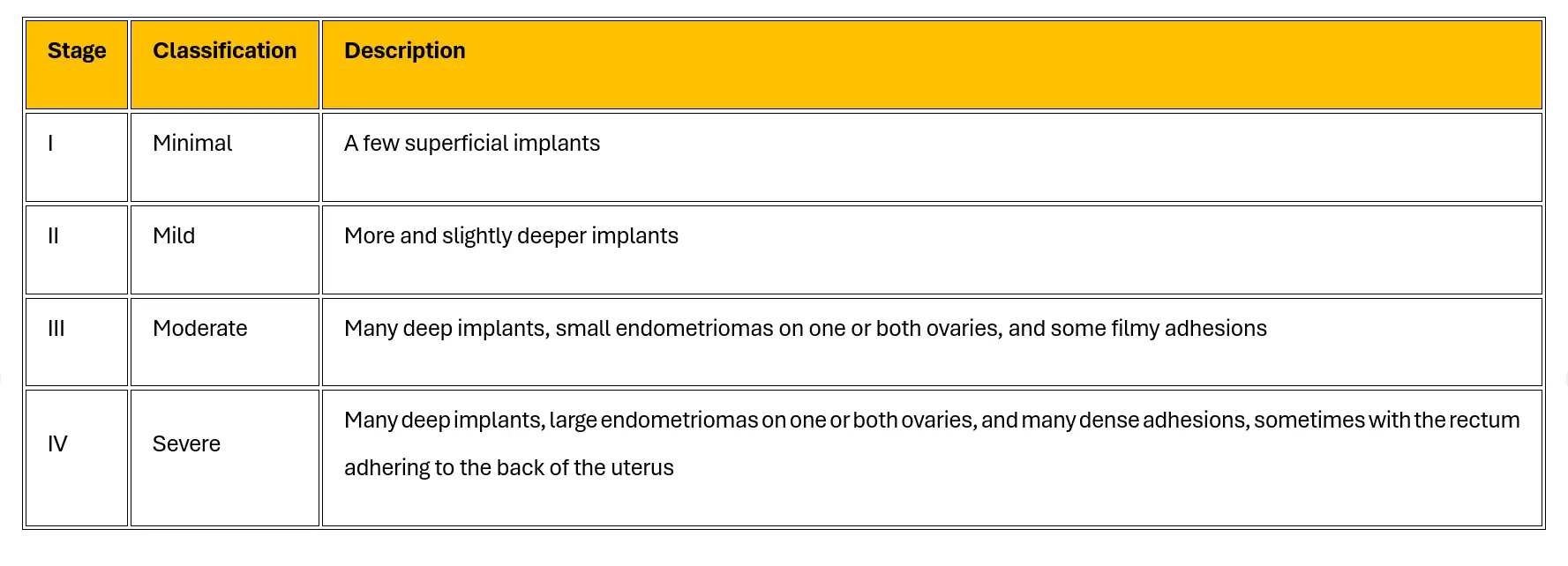
Surgical management options involve cystectomy instead of drainage and coagulation for ovarian endometriomas, minimising ovarian damage. Reproductive surgery can improve pregnancy rates in stages I/II endometriosis (see Table 1).4,6,7
Advanced stages (III/IV), especially deep infiltrating endometriosis (DIE), present complexities. The role of surgery in DIE-related infertility lacks strong evidence, and risks must be weighed.4
Hysterectomy (with or without ovary removal) is an option for those not seeking conception, but its efficacy is not guaranteed. Postoperative use of levonorgestrel-releasing intrauterine system or combined hormonal contraceptives may be recommended for secondary prevention.6
For women living with endometriomas, clinicians should consider ovarian cystectomy instead of drainage and electrocoagulation, weighing the risk of reduced ovarian reserve.6
Post-operative hormone treatment (eg combined hormonal contraceptives) is suggested for long-term prevention of symptom recurrence.6
Regarding alternative options, ESHRE recommends non-medical strategies to address the quality of life (QoL) and psychological well-being of women living with endometriosis. However, no specific non-medical intervention is recommended for pain reduction or improvement in QoL, as their potential benefits and harms remain unclear.6
Importance of fertility preservation
Fertility preservation is essential in endometriosis, and options include embryo, oocyte or ovarian tissue cryopreservation. Vitrification technology for oocyte cryopreservation has shown superior clinical outcomes compared to traditional slow-freezing methods.4
While embryo and oocyte cryopreservation are considered non-experimental, the strength of evidence supporting fertility preservation in endometriosis is limited.4
Subgroups, particularly those with bilateral endometriomas or contralateral recurrence after surgery, might benefit from fertility preservation. Ovarian tissue cryopreservation is an alternative, especially when ovarian hyperstimulation is contraindicated.4
Table 1: Stages of endometriosis7
Conclusion
The impact of endometriosis on women's fertility is intricate and multi-faceted, requiring a comprehensive understanding of its pathogenesis, pathophysiology, and effective clinical management strategies.
The journey towards fertility preservation for women living with endometriosis involves addressing not only the physical symptoms but also the emotional and professional challenges women face.
References
- Gremillet L, Netter A, Sari-Minodier I, et al.Endometriosis, infertility and occupational life: women's plea for recognition. BMC Women's Health, 2023.
- Ballweg ML. The Puzzle of Endometriosis. In Endometriosis, edited by CR Nezhat, GS Berger, FR Nezhat, VC Buttram, and CH Nezhat. New York, NY: Springer, 1995.
- Monnin N, Fattet AJ, Koscinski I. Endometriosis: Update of Pathophysiology, (Epi) Genetic and Environmental Involvement. Biomedicines, 2023.
- Bonavina G, Taylor HS. Endometriosis-associated infertility: From pathophysiology to tailored treatment. Front Endocrinol, 2022.
- Della Corte L, Di Filippo C, Gabrielli O, et al. The Burden of Endometriosis on Women's Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int J Environ Res Public Health, 2020.
- Becker CM, Bokor A, Heikinheimo O, et al. ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum Reprod Open, 2022.
- MSD Professional Version. Stages of Endometriosis. [Internet]. Available at: https://www.msdmanuals.com/professional/multimedia/table/stages-of-endometriosis




